
@ShahidNShah


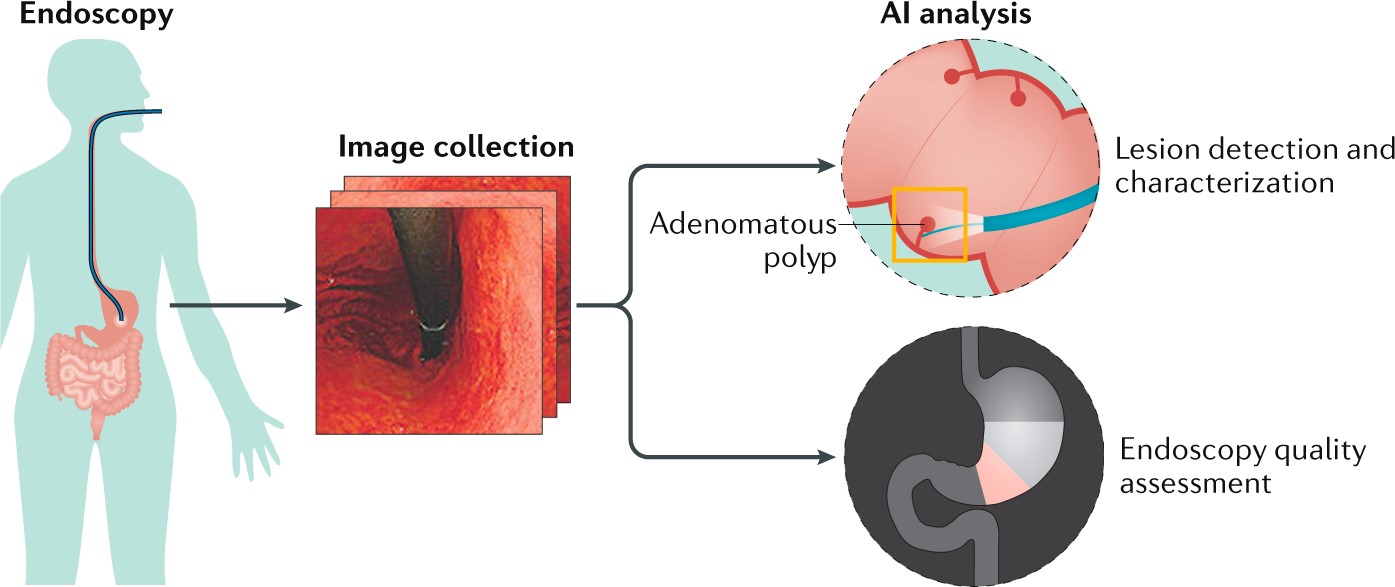
The integration of Artificial Intelligence (AI) into endoscopic procedures heralds a transformative shift in the field of gastroenterology. In the context of medical technology, AI refers to the application of machine learning algorithms and advanced data analytics to interpret, predict, and enhance clinical outcomes through the intelligent analysis of medical data. The advent of AI in this domain is poised to augment the precision of endoscopic analysis, enabling the early detection of conditions such as colorectal cancer and other gastrointestinal diseases with unprecedented accuracy.
Endoscopy, a fundamental diagnostic and therapeutic tool in gastroenterology, involves the use of specialized instruments to visualize the gastrointestinal tract, offering a direct insight into the health of the digestive system. AI and endoscopic technology not only aims to elevate the standard of patient care but also to streamline procedural efficiencies, thereby setting a new benchmark in gastroenterological diagnostics and treatment. As we delve deeper into the implications of this integration, it becomes evident that AI’s role in endoscopy is not supportive but revolutionary.
The inception of AI in gastroenterology can be traced back to the late 20th century when computational methods began to be explored for their potential to assist in the interpretation of medical images. Initial applications were rudimentary, focusing on simple pattern recognition tasks within endoscopic imagery. These early systems aimed to identify specific abnormalities such as ulcers or polyps, setting the stage for more complex diagnostic challenges. Despite their limitations, these pioneering efforts laid the groundwork, highlighting the potential for computational algorithms to augment clinical decision-making.
Key Studies and Technological Breakthroughs
The turn of the millennium brought with it significant advancements in machine learning and computer vision, propelling the application of AI in gastroenterology forward. A pivotal moment in this journey was the introduction of deep learning algorithms, which demonstrated an unprecedented ability to analyze and interpret complex endoscopic data. Studies published in leading medical journals began to report on the efficacy of these algorithms in detecting gastrointestinal lesions, with some findings suggesting that AI could match or even exceed the diagnostic accuracy of experienced clinicians.
One of the most noteworthy areas of application has been in the detection and management of colorectal polyps. Research demonstrated that AI-enhanced endoscopy significantly improved polyp detection rates, a critical factor in the prevention of colorectal cancer.
The Present and Future of AI in Gastroenterology
Today, the integration of AI into gastroenterology represents the cutting edge of medical technology. State-of-the-art AI systems provide real-time assistance during gastroenterology procedures, identifying lesions, and suggesting possible diagnoses, thereby enhancing the accuracy and efficiency of gastrointestinal examinations. Moreover, the convergence of AI with other diagnostic modalities brings in an era of precision medicine in gastroenterology, where treatment plans are tailored to the individual patient based on a comprehensive analysis of their condition.
Colorectal cancer remains a leading cause of cancer-related deaths worldwide, largely because it often goes undetected until it reaches an advanced stage. The detection and removal of precancerous polyps through colonoscopy is a proven method to prevent the development of colorectal cancer. However, the effectiveness of this preventive measure is heavily dependent on the ability to detect polyps of all sizes and types.
AI-Assisted Polyp Detection: How It Works
AI systems designed for polyp detection employ sophisticated algorithms trained on vast datasets of colonoscopic images. These algorithms, leveraging deep learning techniques, are adept at identifying subtle variations in tissue appearance that may indicate the presence of a polyp. Unlike the human eye, which can be subject to fatigue and variability, AI is a consistent, tireless observer that enhances the endoscopist’s ability to detect polyps, especially those that are small, flat, or otherwise difficult to discern.
Evidence of Efficacy
Recent studies underscore the effectiveness of AI in improving polyp detection rates. A landmark study published in a leading gastroenterology journal demonstrated that AI-assisted colonoscopy resulted in a significant increase in the detection rate of adenomatous polyps, the type most likely to develop into cancer. The study highlighted not only the increased detection of polyps per patient but also the ability of AI to identify lesions that had been overlooked in previous screenings. These findings are corroborated by a meta-analysis that pooled data from multiple trials, confirming the superior performance of AI-assisted procedures in polyp detection compared to standard colonoscopy.
Source: https://www.nature.com/articles/s41575-019-0178-y
Implications for Colorectal Cancer Screening and Prevention
The integration of AI into colonoscopy has profound implications for colorectal cancer screening programs. By enhancing the detection of precancerous polyps, AI-assisted colonoscopy can significantly reduce the incidence of colorectal cancer, shifting the paradigm from treatment to prevention. This shift not only has the potential to save lives but also to alleviate the burden on healthcare systems by reducing the need for costly treatments for advanced cancer. The increased detection rates afforded by AI could lead to more personalized screening intervals, optimizing the allocation of healthcare resources.
The Path Forward
The adoption of AI in colonoscopy represents a promising advance in the fight against colorectal cancer. However, the path forward involves addressing challenges related to the integration of AI into clinical practice, including training endoscopists to work alongside AI systems, ensuring the ethical use of patient data, and navigating the regulatory landscape.
As research continues and technology advances, the role of AI in this field is poised to expand.
Barrett’s esophagus, a condition characterized by the abnormal transformation of esophageal lining cells, serves as a known precursor to esophageal adenocarcinoma, a highly lethal form of cancer. The early identification and accurate grading of dysplasia in Barrett’s esophagus are critical for preventing the progression to cancer, yet these tasks present considerable challenges to clinicians.
Diagnosing Barrett’s Esophagus: The Challenges
The diagnosis and surveillance of Barrett’s esophagus involve the detection of dysplastic changes within the esophageal lining, a process traditionally reliant on endoscopic examination and biopsy. This approach is hampered by limitations, including the subjective interpretation of endoscopic images and the potential for sampling error in biopsy procedures. The heterogeneity of dysplastic changes further complicates the detection and grading of dysplasia, leading to variability in diagnosis and management decisions.
The Advent of AI in Barrett’s Esophagus Management
AI models have been developed to address these challenges. In the same manner as the previous example, these models are trained on extensive datasets of endoscopic images, annotated with expert assessments of dysplasia presence and severity. AI algorithms for Barrett’s esophagus detection are trained on endoscopic images annotated for the presence of Barrett’s tissue, including variations in color, texture, and patterns not typically visible to the naked eye. This training helps the AI discern the subtle differences between normal esophageal tissue and areas affected by Barrett’s esophagus.
Through this training process, AI systems learn to recognize the nuanced patterns and features indicative of dysplastic changes, enabling them to identify and grade dysplasia with a level of precision that matches or surpasses that of experienced gastroenterologists.

Potential Benefits for Patient Outcomes
By improving the accuracy of dysplasia detection and grading, AI-assisted endoscopy can facilitate earlier and more targeted interventions, potentially preventing the progression to esophageal cancer. Furthermore, AI can contribute to more personalized surveillance strategies, optimizing the interval between endoscopic examinations based on individual risk profiles. This tailored approach to patient management not only enhances the efficacy of surveillance programs but also reduces the burden of unnecessary procedures on patients and healthcare systems.
Data Privacy and Security
The imperative to protect patient confidentiality stands at the forefront of integrating AI into healthcare. The utilization of patient data, particularly endoscopic images, to train AI models necessitates rigorous adherence to data protection laws. Ensuring the anonymization of patient data and securing it against unauthorized access are paramount concerns that must be addressed through robust cybersecurity measures and compliance with legal frameworks like HIPAA and GDPR.
Training Data and Algorithmic Bias
As we’ve discussed, effective AI models for endoscopy depend on the availability of comprehensive and diverse datasets. The challenge lies not only in amassing a sufficient volume of data but also in ensuring its diversity to reflect the broad spectrum of patient demographics. This diversity is critical in mitigating the risk of algorithmic biases that could compromise the accuracy and fairness of AI-assisted diagnostic and therapeutic recommendations.
Clinician Oversight and the Human Element
Despite the advanced capabilities of AI, the necessity for clinician oversight remains unequivocal. AI is designed to augment, not replace, the clinical judgment of healthcare professionals. The potential for AI to misinterpret data or overlook clinical nuances underscores the importance of maintaining a collaborative relationship between AI technologies and clinicians. This partnership ensures that AI-driven insights are contextualized within the comprehensive clinical understanding, safeguarding against the reliance on AI determinations in isolation.
With its potential to revolutionize early detection and treatment strategies for conditions like colorectal cancer and Barrett’s esophagus, AI promises significant improvements in patient outcomes. However, challenges such as data privacy, algorithmic bias, and the imperative for clinician oversight remain critical to the ethical and effective integration of AI technologies. As the field progresses, continued collaboration and innovation will be key to realizing the full potential of AI in improving gastroenterological health outcomes, heralding a new chapter in medical practice.

Chief Editor - Medigy & HealthcareGuys.
Alcohol addiction remains one of the most challenging public health issues, affecting millions globally. Jalie A. Tucker (2020) reports that approximately 14.5 million Americans aged 12 and older had …
Posted Feb 27, 2024 Rehabilitation Addiction
Connecting innovation decision makers to authoritative information, institutions, people and insights.
Medigy accurately delivers healthcare and technology information, news and insight from around the world.
Medigy surfaces the world's best crowdsourced health tech offerings with social interactions and peer reviews.
© 2025 Netspective Foundation, Inc. All Rights Reserved.
Built on Apr 17, 2025 at 6:07am